What are Venous Ulcers?
Venous ulcers, also known as venous stasis ulcers, represent the most severe symptoms of chronic venous disease, characterized by open wounds on the legs that either heal poorly or not at all. They are classified as the final severity group C6 on the CEAP classification scale.
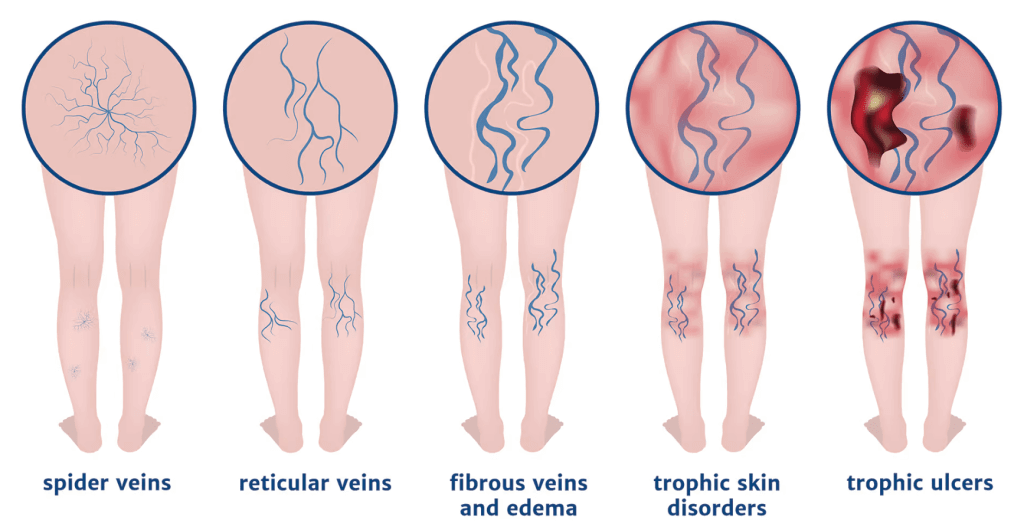
CEAP classification is a widely used method for classifying and grading chronic venous disorders. The scale ranges from (C0), no visible or palpable signs of venous disease, up through spider veins (C1) and varicose veins (C2) to active venous ulcers (C6). CEAP stands for Clinical, Etiologic, Anatomic, and Pathophysiologic, representing the key components considered in the classification.

Causes of Venous Ulcers
Venous ulcers can arise from all forms of chronic venous disease, with chronic venous insufficiency being the most common cause. Venous insufficiency is when the normally blue, healthy veins start failing to adequately return blood to the heart, leading to blood pooling in the legs. When the valves in the veins in your legs malfunction, gravity takes over and keeps some of the blood from returning to the heart. This results in chronic leg swelling and venous hypertension, leading to inflammation of the skin. Over time, the inflamed skin cannot withstand the ongoing damage, resulting in the formation of open wounds.
Other causes of venous ulcers include deep vein thrombosis (DVT) and May-Thurner Syndrome, both of which can cause venous hypertension and hinder proper blood flow. Diagnosing these conditions can be easily overlooked and requires an experienced vascular surgeon to diagnose and provide treatment.
Risk Factors for Venous Stasis Ulcers
Risk factors for developing venous ulcers include family history, female gender, advanced age, obesity, physical inactivity, prolonged standing, peripheral arterial disease, and a history of venous blood clots (DVT) or post-thrombotic syndrome.


Symptoms of Venous Stasis Ulcers
Venous ulcers typically present with obvious symptoms. The open wounds on the legs are often painful and sensitive to touch. Surrounding areas may exhibit signs of chronic inflammation, such as redness. Additionally, the wounds may be covered in a thick, yellow substance called biofilm, which is a layer of bacteria on the skin’s surface.
Complications that come from venous ulcers always being exposed to skin bacteria can include infections such as cellulitis and sepsis. In rare cases, extreme infections can lead to limb amputation or death.
Treatment of Venous Ulcers
Diagnosis and treatment of venous ulcers may be complex, but you do not have to navigate it alone. Our board-certified Fox Valley Surgical vascular surgeons are trained to diagnose and manage this condition effectively. If you are experiencing chronic venous disease and venous stasis ulcers, do not hesitate to seek professional medical attention. Prompt treatment is essential to prevent ulcer recurrence and improve overall health and well-being.
Treatment for venous ulcers requires a comprehensive approach:
Wound Care
Proper wound care, including regular cleaning and appropriate dressing, is essential for preventing infection and facilitating healing. If a wound is not clean, the body responds by walling-off the bacteria rather than closing up the wound.
Compression
Compression therapy through stockings or dressings is part of the treatment of venous stasis ulcers. Compression helps reduce skin swelling and inflammation, addressing the underlying mechanisms contributing to wound development.
Venous Disease Treatment
Addressing underlying venous and arterial diseases is crucial for effectively managing venous ulcers. Your vascular specialist will evaluate your entire vascular condition and not just the treatment of the ulcers.
Lifestyle Modifications
Adopting a healthy lifestyle, including weight loss, increased physical activity, and other healthy habits, can promote healthy circulation and facilitate wound healing.
Medications
Antibiotics may be prescribed to control wound or skin infections. Pentoxifylline, a medication with microcirculation properties, may be used alongside compression therapy to enhance healing rates. In some cases, steroids may be utilized to reduce skin inflammation and promote wound healing.







