MAY-THURNER SYNDROME
What is May-Thurner Syndrome
May-Thurner Syndrome (MTS), also known as Iliac Vein Compression Syndrome, is a relatively rare yet potentially severe condition affecting the veins in the pelvis. It occurs when the left iliac vein becomes squeezed or compressed by the neighboring right iliac artery, potentially leading to back-pressure in the leg.
The syndrome was first identified in 1851 by Drs. May and Thurner, hence its name. It is not a particularly common disease and is believed to be under-diagnosed and under-treated in the medical community.
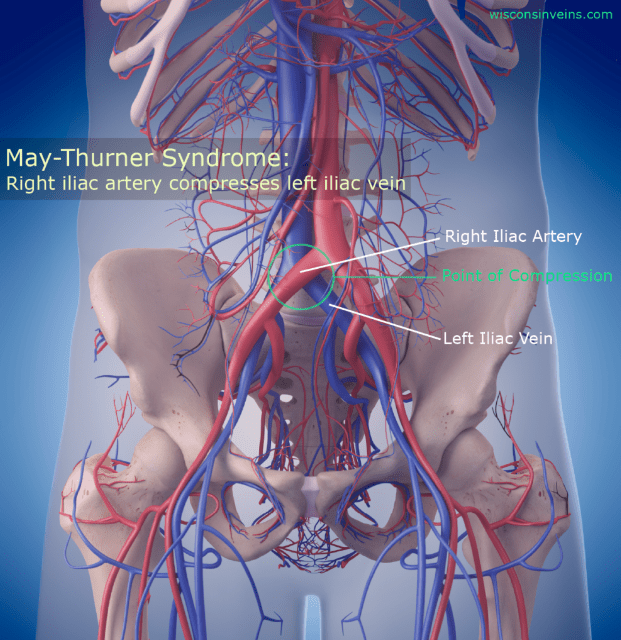
Illustration of May-Thurner Syndrome
Causes of May-Thurner Syndrome
In human anatomy, the major pelvic veins known as iliac veins serve as crucial pathways for blood returning from the legs to the heart. These blue veins naturally lie between the spine and arteries, with some level of compression being typical.
However, when this compression becomes exaggerated, it can cause May-Thurner syndrome. While the left leg is most commonly affected, the condition can also impact both legs.
Symptoms of May-Thurner Syndrome
Symptoms of May-Thurner vary, ranging from mild discomfort to complications such as severe blood clots. Many patients experience one-sided leg pain and swelling, often misdiagnosed for years. Over time, chronic back pressure from MTS may cause varicose veins, chronic venous insufficiency, skin pigmentations, and ulcers. In severe cases, the compression can restrict blood flow, resulting in blood clots known as iliofemoral deep vein thrombosis (DVT).
MTS is frequently seen when we are treating acute illnesses or trauma. The additional stress on the body can cause the blood to thicken which decreases the blood flow through the compressed iliac vein. MTS is more prevalent in women and commonly occurs in individuals aged 20 to 50.
Diagnosing May-Thurner Syndrome
MTS can be diagnosed through various methods. Initial assessments typically involve venous ultrasound of the legs to assess downstream effects. The ultrasound does not usually image the iliac vein directly, it can direct the physician to look at other causes.
Imaging studies such as CT or MRI scans of the abdomen and pelvis are a good way to see the iliac veins and detect MTS. Formal venography with intravascular ultrasound is considered the gold standard diagnostic test for MTS.
Treatment of May-Thurner Syndrome
The vascular surgeons at Fox Valley Surgical Specialists have a variety of treatments for MTS. Compression stockings are often recommended initially to alleviate swelling non-surgically.
Procedural steps that most physicians will follow to relieve iliac vein compression are:
- Diagnostic Venogram - a large IV with an imaging camera is inserted into the leg vein to allow the physician to see a live view of the iliac vein. This is usually done in combination with an IV contrast injection and an ultrasound probe called an intravascular ultrasound (IVUS).
- If clots are detected, the surgeon can use a number of clot-clearing techniques such as administering clot-dissolving medications, suction removal, or dragging a clot retrieval device across the clot.
- Once the clot is cleared a stent may be placed in the vein to help the vein stay open and reduce the possibility of future compression.
- In rare cases, when the above techniques are not effective, the surgeon may perform a bypass around the affected area.
Your Experienced Vascular Team

Robert Ballard, MD



